Learning to walk after a spinal cord injury
This is a case of a 65 year old healthy woman who fell from 7 steps and experienced loss of consciousness for a few minutes. As a result of the fall, the woman sustained a C7 cervical spinal cord injury (SCI).
The patient's injury was classified as ASIA A and she had to undergo cervical spinal fusion after the injury. She received basic rehabilitation at the hospital and experienced a few complications, such as pneumonia and a urinary tract infection during her hospitalizations. She later came to our facility for neuro rehabilitation.
Evaluation
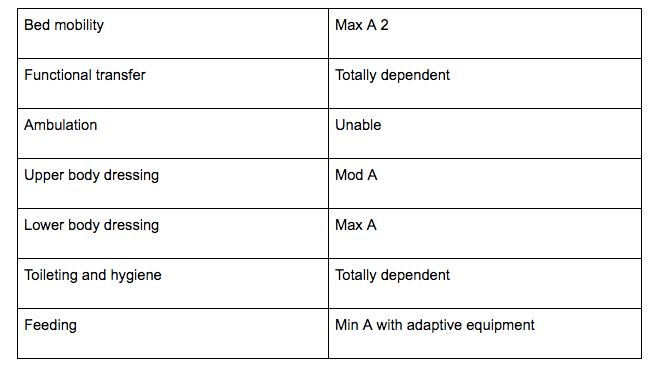
The patient's status at the time of evaluation was as below:
The patient went through aggressive physical and occupational therapy for 5 to 7 days per week for almost a year and a half after her injury.
Results
This patient experienced improvement with the plan of care. She demonstrated more improvement in the upper extremities than she did in the lower extremities. Also, her left leg was weaker and had less voluntary control compared to her right leg and arms.
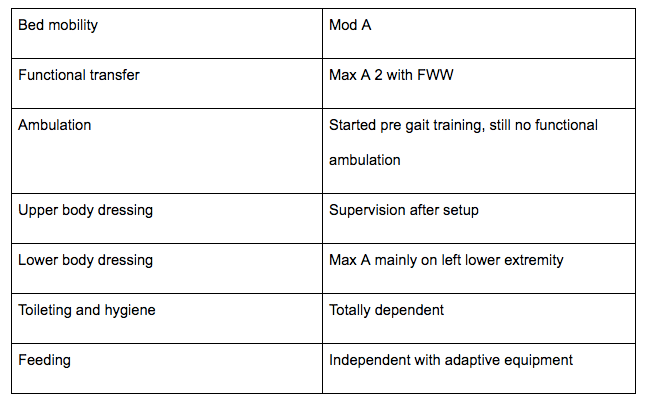
After 8 months of aggressive rehab, her functional status was as below:
Gait training
Gait training was the most difficult task for this patient.
The MMT on the left leg showed the following results:
Hip abductors: 1/5
Hip flexors (group): 2+/5
Hip extensors: 1/5
Knee extensors: 3/5
Knee flexors: 3+/5
Ankle dorsiflexors: 0/5
Ankle plantarflexors: 3/5, resulted in foot drop during pre gait training
Putting it all together for functional ambulation
As you can see from the MMT scores above, the main muscles that act during the gait cycle are either very weak or not turning on at all. In other words, these muscles are not firing or generating enough force for the gait cycle.
The right leg demonstrated at least 3/5 strength for all major muscle groups. Therefore, when my patient stood up with the walker, she could advance her right leg while I supported her left knee to prevent sudden buckling. However, she was not able to advance further than this.
At that point, I had to put her on the mat again and start with basic neuro facilitatory techniques to activate the hip flexors, hip extensors, and hip abductors. I started with the gravity eliminated plane first. I also used neuro re-education with electrical stimulation to passively activate those big, bulky muscles (hams, quads, glutes, etc).
After 2 weeks of this regimen, I did not have to support the patient's left knee when she advanced the right leg when she used the walker. However, she was still unable to advance the left leg independently.
I could feel her activating the hip extensors and abductors, but she was unable to perform hip flexion, knee extension, and ankle dorsiflexion simultaneously to advance the leg for heel strike. She could only perform hip flexion, knee flexion, and ankle plantarflexion.
Use of wrap, brace, and splint - being creative!!
I decided to start wrapping the patient's knee to prevent knee flexion and I applied tubi grip (the small sock like material on top of the gripped sock) to “slide” the heel easier with foot drop. I also passively performed hip flexion (ACE wrap will keep the knee in extension and the tubi grip will allow me to slide the heel on the floor easily). The patient was then able to advance her leg!
We continued to do the same exercise almost daily after we completed the strengthening and mat exercises. In a week or so, she was able to walk 50 feet with me just “pushing/sliding” her hip a little bit to initiate hip flexion. I was essentially providing moderate assistance for gait training with a walker.
Since my patient was now more stable on her feet, I started using a knee brace (it was a double upright drop lock) on her left leg. With the use of a knee brace, she was able to perform hip flexion with a little hip hiking while keeping the knee extended.
This allowed her to clear the floor and advance the left leg since she did not have a heel strike response due to her foot drop (the foot drop was not severe though; she was able to actively bring the ankle to neutral, but was not able to perform any dorsiflexion).
Now as a clinician, I knew that we needed to keep strengthening hip abductors and hip extensors while continuing to try to activate the ankle dorsiflexors on the left side. Also, daily repetition of the gait cycle was helpful. Consistent practice strengthens the neural connection and allows the patient to reproduce the same movement easily.
Currently, this patient is not receiving any skilled physical therapy, but she ambulates using a front wheel walker with supervision from the nursing staff. She does not need any braces or support to perform ambulation!
This was a great achievement for my patient. After her injury, she was unable to move her legs and was not sure if she would ever stand or walk again. With aggressive and consistent skilled physical therapy, we were able to achieve excellent results.
Conclusion
After SCI (especially ASIA A), it is very difficult for a patient to remain positive and believe that he or she will get back to walking. PTs need to use different approaches in order to find out what works for each patient. It is also important to believe in yourself as a clinician. Your attitude will help shape your patient's attitude.
At times, rehab from a SCI can be depressing and your patients may want to give up at some points. As a clinician, you may not be sure if you can achieve your patient’s goals, but you can be certain that you are providing the best PT possible.
You also need to provide psychological support, positive thoughts, and motivation to your patients. When you and your patient are working as a team toward the same goal, it becomes “easier” to be a therapist and you are more likely to think critically to achieve “that goal."