“Extensive research has shown that no matter how knowledgeable a clinician might be, if he or she is not able to open good communication with the patient, he or she may be of no help.” (Hulme et al., 1988)
Health care has not always been recognized as the team effort that it is today. In the “old days”, people were cared for by one all-knowing doctor who lived in the community, visited the home, and was available to attend to needs at any time of day or night. In this new age of health care reform, rehabilitation medical teams consist not only of the MD, but also a number of rehabilitation therapists (PT, OT, ST, nurses, recreational therapists, and social workers). The goal of the rehabilitation medical team is to help maintain high quality care for all of their patients. As a result, there has been an influx of research showing improved outcomes with a team approach (Hulme et al., 1988). In order for any team to be successful, the members must understand the value in communicating relevant information.
However, the development process of physical therapists does not always prepare them adequately for the realities of communication within the changing health care system. After graduation, new therapists may recognize that there can be a disparity between their training and what is expected of them in practice. In the past, the therapist was a practitioner who followed specific physical therapy prescriptions from physicians. Now, therapists are trained to be independent professionals who evaluate the patient's needs, design an appropriate treatment plan, and monitor the effects of the treatment. If a treatment plan does not solve the patient's problems, the therapist assumes a greater role in developing alternatives. In practice, physicians often times delineate the boundaries of responsibility and autonomy for physical therapists in delivering optimal patient care. The process is both direct and implied. How does a physical therapist respectfully communicate his or her own treatment plan prerogatives instead of blindly following the prescription? Outlined below are 5 tips to help improve a newly graduated physical therapist's ability to communicate his or her own goals and thoughts with other members of the rehabilitation medical team.
Tips for Communicating with Physicians
1. Be Prepared
Communicating with a physician, on behalf of the patient/client, is an ability that can be one of the paramount reasons the patient/client has better outcomes. At the base of all communications, there are facts and pieces of data that we, as physical therapists and clinicians, extrapolate from our patients. As increasingly autonomous practitioners, PTs are able to perform ongoing assessments to determine the diagnosis, prognosis, and any need for referrals to other healthcare practitioners (Hulme et al., 1988). As any self-help book or philosophy guru would say, “knowledge is power.” In the seemingly endless deluge of research papers and evidence, it may seem daunting to stay up to date with the newest treatment approaches. However, if we want to be taken seriously as autonomous clinicians, we must go above and beyond mediocrity to push the profession into the limelight. All professionals are prepared. The more prepared you are, the better your chance for success. For instance, a dentist reviews your chart before pulling out the picks and drills. Lawyers brief together before entering a courtroom. Can you imagine any of these professionals going about their daily routines without being prepared? The same goes for your clients and their physicians. Do your homework. Study the patients' charts. Read up on new research. Go over old notes from school or peruse a textbook. A physician hopefully will not only respect the time and effort you put into the patient, but you may even provide vital information of which the physician was not aware. This gives you a bond in knowledge. Potentially, this trust may lead to the physician providing you with more referrals in the future. Ultimately, this should provide you with an open channel of patient-centered dialogue. Do not go in blindly. Depending on the method of communication (phone, email, letter, etc. covered in #4) always have notes prepared, whether they be talking points, references for the physician, patient data, and or data from previous patient experiences. This will help you stay organized and on point, and be able to offer concrete suggestions. Hulme et al. (1988) specifically states that physicians will show more interest if conversations are purposeful, direct, and supported with concise facts.
2. Listen

The cornerstone of communicating is the ability to listen, and in our fast-paced society, genuine listening has become a rare gift. It helps build relationships, solve problems, ensure understanding, resolve conflicts, and improve accuracy. Listen without judging the physician or criticizing the things he/she tells you. If what is said alarms you, go ahead and feel alarmed, but don’t say to yourself, “well, that was a stupid move.” As soon as you indulge in judgmental bemusements, you’ve compromised your effectiveness as a listener. Listen without jumping to conclusions. Remember that the speaker is using language to represent the thoughts and feelings inside his/her brain. You don’t know what those thoughts and feelings are, and the only way you’ll find out is by listening. As Hulme et al. (1988) points out, newly graduated physical therapists can improve communication skills by maintaining assertiveness without aggressiveness. This includes the ability to maintain stability in the conversation, follow the flow, and do not interrupt for the sake of interruption. Predict the lull in their response and then use that to iterate your thoughts. We all think and speak at different rates. If you are a quick thinker and an agile talker, the burden is on you to relax your pace for the slower, more thoughtful communicator or for the person who has trouble verbally expressing him or herself. As we learned in PT school, while taking a patients' history, repeating what has been said for clarification is an immediate way to show you have been listening and are engaged in the conversation. DO NOT ZONE OUT. This is not a conversation with one of your college friends; this is a professional situation with a person’s health on the line.
3. Have Confidence
In the purest sense, confidence is understanding your talents, the value you provide, and acting in a way that conveys that to others. Contrast this with arrogance or low self-esteem. The former typically involves believing you are better in a particular area than you are, while the latter involves believing you're less valuable than you are. The closer your self-assessment is to reality, and the more you behave accordingly, the closer you are to displaying healthy confidence.
According to Hulme et al. (1988), recent graduates and student physical therapists were reluctant to open lines of communication through the telephone because they were afraid of being wrong or appearing to not to know what they are talking about. However, refraining from doing so feeds the hierarchical structure in which the sole decision-making responsibility lays in the physicians hands. In this same study (Hulme et al., 1988), experienced physical therapists relayed that these recently graduated therapists and students should not be intimidated by the referring physician and should seek out communication channels. Here are ways to help you overcome this fear.
- Emphasize strengths by giving yourself credit. Take a look at your track record, what have you accomplished during your school career in regards to social interactions, presentations, and past clinical rotations completed. Why should this be any more difficult than evaluating a new patient?
- Take a risk by looking at this new experience as a chance to learn, not win or lose.
- Use positive self-talk by stopping in the middle of a negative thought, and re-framing it with positive thoughts or words.
- Practice self-evaluation to gain a stronger sense of self. This will help prevent you from giving away your personal power to others.
Competent practice makes perfect. As with any skill set, one must actually perform the task to learn how to perform it well in the future. Don’t be afraid of making mistakes. You will make some mistakes, and that’s okay. You learn from them and keep going. Confidence is a skill that develops with awareness and practice. Think of confidence as a sports skill. If you practice bad technique repeatedly, you will become very skilled at the bad technique and that is what will come out during game time. Though your confidence may wax and wane, find people in your life who you can count on to give you a "booster shot" of confidence; for example, have your boss say, "I know you can do it" or a friend tell you, "Hang in there. Things will turn around."
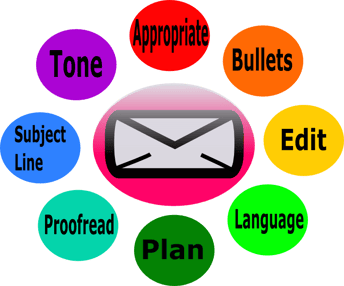
4. Mind your form of communication
Today, the advancement of technology allows us a boundless array of ways to communicate. From social media to cellular phones, email, video and more, we're expected to be in constant communication with each other. As a result, new technologies have the power to enhance, but also can hinder our communication style. How can PTs use new forms of communication appropriately, to foster better relationships with physicians and patients?

Email -There’s no doubt that we live in an increasingly electronic world, but the latest numbers from the Pew Research Center’s Internet & American Life Project make it clear: 85% of Americans are online (2012b, para. 1). 55% of US adults go online wirelessly (2012c, para. 1). Emails are not always the most appropriate form of communication. Ask yourself, "Is this a potentially sensitive message that may be misunderstood if relayed through email?" If you’re struggling to convey emotion or tone in your email, it might be better to pick up the phone (TeamSTEPPS).
However, there are times in which some physicians use this as a form of communication not only with their patients but with other healthcare practitioners. Physicians of the younger generation seem to be more inclined to use this method of communicating because society as a whole is becoming more attuned to the online world. The speed and ease of which one can use this technology has progressed wildly over the last 10 years (Smith, 2016). Furthermore, it seems healthcare practitioners are frequently checking their email during the work day instead of their office's voicemail. It may behoove you to ask your patient how their doctor communicates with them and that may clue you in to how you should contact the patient’s physician. For example, 80% of patients in a family practice clinic expressed interest in email communications. Most reported that their email address changed less frequently than their home address or telephone number (Virji et al., 2005). Email provides a written record of the exchange and enables either the physician or physical therapist to focus on questions they want to ask and ask follow-up questions. Rather than trying to recall healthcare provider’s answers from an in-person or telephone conversation, they can review the written reply at any time. DO NOT USE ANY SLANG OR TEXT LINGO SUCH AS “LOL” OR “OMG”. It screams lack of professionalism. Imagine this is a hand written letter and use appropriate introductions and sign offs such as “Dear Dr. Jane Doe” or “sincerely” respectively. Usually, at first contact, it is wise to use a more professional introduction. If you have been able to communicate with the individual over several emails, it is okay to change to a more congenial but respectful introduction of “Hello, Doctor”. Unless stated by the physician, do not call them by their first name. Many times there are egos involved and just because they might not reciprocate, do not assume that they do not respect you (this can be a whole other discussion) (Weaver et al., 2012).
Texting - In a business context, texting should be kept to a minimum, if used at all. It might be appropriate if your clinic or hospital provides an inter-professional messaging system like SMS. In acute settings, physicians also may initiate texting. Otherwise, do not use or initiate the use of this method (Ravenscraft, 2015).
Telephone -You might be experienced at talking on the phone, but in addition to a pleasant phone manner, practicing good mobile phone etiquette will help you get more value out of conversations. When speaking on the phone, ensure that you remain focused on the person on the other end. They will know if you are multitasking while talking – whether you’re checking emails, washing dishes, or on your way from A to B. A person’s distraction can be heard in their voice. Set aside time to make phone calls so you can devote your whole attention to the conversation. For voicemail, leave a concise message about what you need, by when, and try to keep the voicemail to less than 60 seconds if possible. If the physician calls and you are with a patient at the time make sure to return their call promptly, either same day or next. This shows respect and also effort (Weaver et al., 2012).
Conference Calls - Be on time; set a reminder on your phone if you think you'll forget. Use a good quality headset. Avoid a wireless headset because of the added complications of battery and wireless connection. Mute yourself when you're not speaking and position your microphone so that the others don't have to hear your every breath. You may want to invest in a noise-canceling headset unless you can consistently use a quiet room. Be concise in your comments and don’t dominate the call. Make sure to let others get their thoughts out too. Speak slowly and clearly if the call includes international participants. Don’t use a cell phone if your connection is weak. In fact, don’t use a cell phone at all, if you can avoid it, as the short delays inherent in modern digital cell transmissions make back-and-forth discussions very difficult (Weaver et al., 2012).
5. Ask for help

It takes a strong person to ask for help in the professional world. Many of us have fallen for the myth that asking for help is a sign of weakness. In reality, asking for help is the brave thing to do. Used judiciously, this will make your relationships more authentic, balanced, and intimate. This could mean pursuing a conversation with one of your more experienced peers, the director of your clinic, or any senior staff. They too were once new, and many of them have formed relationships with physicians, thereby creating sources for referrals and other collaborative efforts. We all have struggles and we’re not able–or meant–to face them alone. Most newly graduated clinicians are surrounded by people who would love to lend them ear or a little advice. All you have to do is ask. Every person has had different experiences, follows a different thought process, and has their own way of approaching life; don’t discount the power of getting someone else’s perspective on what you’re going through. Plus, sometimes you’ll find you didn’t even need a solution at all, you just needed to talk. I have found that the profession of physical therapy has fostered a group of individuals who, for the most part, want to help one another (Hulme et al., 1988).
For Future generations of physical therapists, the education curriculum should include not only aspects of patient communication, but communication with physicians and other healthcare providers, as well. As a student, I was not afforded that opportunity as often as needed. As I have heard with others, some CI's (also clinic owners) would rather be the communication point with the physician to help foster the clinics relationship rather than the students education. Also, many clinics have weekly journal club and/or presentations. These clinics should find time to improve each of their clinician's ability to communicate to physicians through workshops or other mentoring programs (Hulme et al., 1988).
Have Questions? Leave a comment below and we will get back to you ASAP!

